The Threat Bucket Update Vol 2.
Jun 18, 2025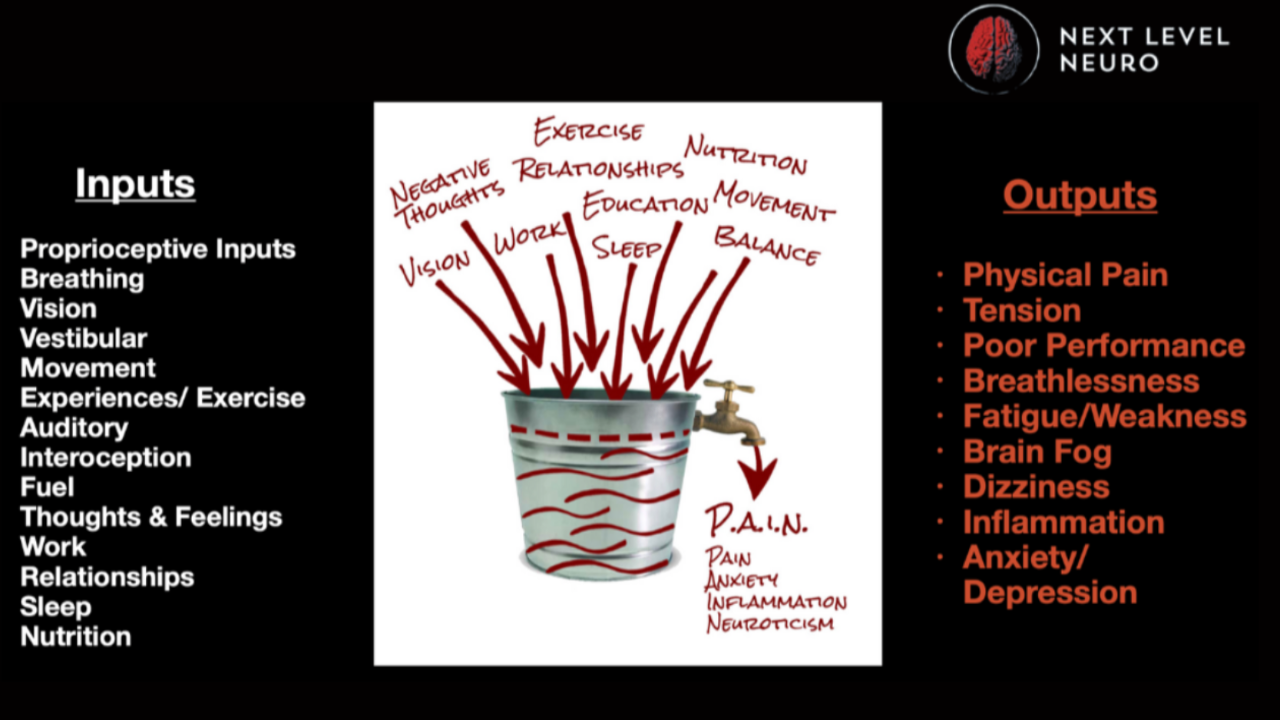
How the Brain Interprets Stress — And Why the "Threat Bucket" May Be the Missing Piece in Your Client Care
“You need to reduce your stress.”
Heard that one before? Maybe you’ve even said it to a client.
How many of you have thought your clients' lifestyle factors were/could be responsible for their lack of success (success being pain etc), but you only say that AFTER you have tried every biomechanical trick in your book?
It’s good advice. Of course, we need less stress, better sleep, less stress and a whole litany of lifestyle changes.
But here’s the problem: no one tells you how to do that, especially when your knee’s been hurting for 8 years, your job feels like emotional quicksand, and you haven’t had a real night of sleep since your kid was born.
This is where the Threat Bucket comes in. And it is something we teach Day 1, sentence 1.
It’s a model that changes everything, from how you understand pain to how you structure your assessments, training sessions, and client care plans.
This isn’t just a clever metaphor.
It’s a brain-based framework for helping your clients move, feel, and live better.
What Is the Threat Bucket?
Imagine your brain has a bucket.
All day long, it collects information from inside and outside the body—what neuroscientists call inputs.
These inputs include:
- Old injuries
- Emotional trauma
- Poor sleep
- Gut inflammation
- Visual system fatigue
- Unprocessed grief
- Financial pressure
- Food sensitivities
- Unstable joints
- Childhood adversity
- Daily micro-stressors (e.g., loud noise, scrolling social media, arguments)
And your brain doesn’t separate them neatly. It doesn’t file “work stress” under one tab and “ankle sprain” under another.
It just asks one question: “Are we safe?”
And if the answer is “not really,” it starts to fill the bucket.
So what happens? We all have these types of things in our lives, right?
When the Bucket Overflows: Pain, Fatigue, Anxiety, Shutdown, etc
Your nervous system is designed to keep you alive, not optimized.
When the threat bucket gets too full, the brain pulls the emergency brake.
That emergency brake might show up as:
- Chronic pain that has no biomechanical cause
- Migraines or brain fog
- GI distress
- Panic attacks
- Insomnia
- Emotional reactivity
- Postural compensations
- Fatigue that sleep doesn’t fix
In applied neurology, we call these outputs signals the brain uses to slow you down, limit risk, or trigger protective patterns.
Pain is not the problem.
Pain is the brain’s solution to an overloaded system.
***REREAD THAT LAST SENTENCE****
Is it that important, YES!
Threat Is Threat: Your Brain Doesn’t Distinguish
This is the single most important principle we teach in our programs:
The brain treats all forms of threat equally.
Pain is pain. Stress is stress. Emotional or physical—it’s all the same in the nervous system.
This is why your client’s shoulder hurts more after a breakup.
Why their chronic back pain flares when they haven’t slept.
Why they regress after a high-stakes performance review at work.
The brain doesn’t care whether the input is a tight psoas or a toxic in-law.
If it perceives threat, it fills the bucket.
So, how do we empty the bucket?
The Spout: How the Brain Tries to Regulate
Let’s go back to the bucket. The only way to stop it from overflowing is to give it a working spout—a way to drain stress and restore balance.
The brain does this automatically by adjusting outputs:
- It may shut down muscle function.
- It might reduce range of motion.
- It might trigger a pain loop to keep you still.
- It might flatten affect or increase anxiety.
Your job as a coach or therapist isn’t just to empty the bucket—it’s to restore the spout.
That means:
- Reducing threat where you can
- Improving inputs (like sensory integration, breath, visual drills)
- Supporting the nervous system so it feels safe enough to stop reacting
And this is where Applied Neurology is the center of that bucket and adjusting that spout.
Applied Neurology: Rewriting the Threat Bucket
In applied neurology, we take this model and use it.
We train professionals to identify what’s filling their clients' threat bucket and give them tools to drain it before it overflows.
Here’s how that might look in session:
Assessment
Instead of just looking at the site of pain (e.g., a hip impingement), we assess:
- Visual and vestibular stability
- Breath quality
- Gait and proprioception
- Sensory mismatch
- History of trauma, surgeries, or stress
Reassessment
We apply a brain-based drill (like a balance input, vision reset, or cranial nerve activation), and check:
- Range of motion
- Strength
- Pain levels
- Emotional affect
- Neurological response (flinch reflex, eye tracking, gait)
If the response improves, the threat is lower.
If it worsens, the threat is higher.
This is how we let the nervous system guide the plan.
Real-Life Example
When the Pain Isn’t What You Think
Client: 42-year-old woman, ex-athlete, reports persistent knee pain.
History: ACL surgery at 27. Pain comes and goes. Gets worse with stress.
Typical rehab approach: Strengthen quads, glutes, improve hip mobility.
Client result: Mild improvement, pain returns under pressure.
Neurology-first approach:
- History shows vision issues (convergence insufficiency).
- Testing reveals instability with eyes closed.
- Introduce eye-tracking drills + vagus nerve stimulation.
Result:
Pain decreases by 40% in 5 minutes.
Knee range of motion improves.
Client reports, “I feel more grounded.”
Assess and Reassess show positive results.
Why?
We addressed a threat input that was overfilling the bucket, not the tissue itself.
What’s Filling Your Client’s Bucket?
Here’s a breakdown of common stressors that fill the threat bucket—and how you might identify or address them.
|
Input Type |
Examples |
Applied Neuro Approach |
|
Physical Injury |
Old sprains, surgeries, concussions |
Joint mapping, gait analysis |
|
Sensory Dysregulation |
Poor vision, vestibular dysfunction, balance loss |
Eye drills, head movements, proprioceptive work |
|
Emotional Trauma |
Grief, fear, PTSD |
Vagus nerve work, safe environment, sensory grounding |
|
Metabolic Stress |
Inflammation, food intolerance, dehydration |
Hydration, anti-inflammatory habits |
|
Cognitive Overload |
Work stress, multitasking, overwhelm |
Breath retraining, visual resets, movement breaks |
Pain Science Meets Practice
You’ve probably heard of the biopsychosocial model of pain.
It emphasizes:
- Biological injury
- Psychological factors
- Social/environmental influence
But here’s what most approaches miss:
All of these are interpreted by the brain.
Because without understanding how the brain processes threat, you’re missing the master key.
The Future of Client Care Starts Here
If your assessments only look at biomechanics…
If you treat pain only where it shows up…
If you ignore visual, vestibular, or emotional inputs…
Then you’re working downstream from the brain.
The Threat Bucket shows us why people don't get better even when they do everything “right.”
It shows us where the system breaks down.
And more importantly, it shows us how to build it back up.
Practical Takeaways for Coaches & Therapists
- Start Every Session With Nervous System Input
Use sensory drills, breathwork, or vision resets before loading the body. - Ask: What’s Your Client’s Stress Capacity Today?
On high-threat days, back off loading and prioritize regulation. - Use Reassessment
Test, apply a neuro drill, retest. Let the brain tell you what’s working. - Don’t Ignore “Weird” Symptoms
Gut issues, migraines, emotional dysregulation, they’re all signs the bucket is full. - Track the Spout
If a client responds poorly to an input, it’s not a failure; it’s feedback.
Stress Isn’t Going Away
You can’t eliminate stress.
But you can change how your brain interprets it.
And when you do, you unlock performance, healing, and a sense of agency that biomechanical approaches just can’t reach.
That’s what the Threat Bucket gives us: a map.
A way to navigate the complexity of being human.
Let’s stop chasing pain and start listening to the brain.
If you want to learn more about our assess-reassess process, here are 3 FREE masterclasses on it.
Want more information on our Mentorship and Programs?
We hate SPAM. We will never sell your information, for any reason.

